在二月的一个下雪天,克里斯汀·梅耶突然意识到自己必须亲自负责宾州的疫苗接种工作。
内科医学医师梅耶在宾州费城郊区的艾克斯顿拥有一家20000病患的医院。数周以来,他一直在接听病患的电话,这些病患拥有注射新冠疫苗的资质,但无法在药房、医生办公室,或通过当地卫生部门以及州疫苗信息网站进行预约。大多数病患的岁数都超过了75岁,而且很多人难以通过各大系统在线进行注册,因为这些系统对于科技设备操作的熟练度有很高的要求。
当暴风雪来临时,梅耶取消了个人就诊预约,并要求其医师和员工在日间帮助病患注册疫苗接种。她在其医院的Facebook页面上发布了贴文,在两个小时内,有1200人向她的办公室发送邮件寻求帮助,医院服务器也因此而瘫痪。不久之后,梅耶在Facebook上创建了一个由志愿者经营的匹配服务,以便让高龄人士或其孩子或邻居,获取找寻接种服务的帮助。截至3月底,这个组织的成员超过了6万人(包括在宾州长大、身为记者且尝试帮助其当地父母接种疫苗的我本人)。当时,很少有用户在等待州发布的消息:论坛上讨论的内容全是沃尔格林(Walgreens)、CVS、Rite Aid和其他药房什么时候才会批量公布接种预约机会,以及如何最为高效地使用其通常令人抓狂的预约网站。
梅耶通过视频向《财富》杂志透露:“说真的,疫苗接种事务让我感到心力交瘁。”她的语速和手势逐渐加快,并透露出一种沮丧情绪。“我把所有的希望和所有病患的希望都寄托在了卫生部门的身上,因为事情本该如此,然而这个流程出了问题。”
梅耶和数百万宾州民众意识到,宾州的疫苗接种问题远非令人困惑的注册流程那么简单。拥有超过2.48万家医院的宾州是全美新冠疫情死亡人数排名第五的州,同时也是美国疫苗接种问题最严重的州之一。《贝克尔医院评论对疾控中心数据的分析显示,在1月底,宾州收到了近200万剂疫苗,但仅接种了42%,在美国排名第49位,仅位于阿拉巴马之前。该州240万老年易感人群一直在想方设法获取疫苗接种服务,然而,该州却向儿科医院发送了1.2万剂疫苗,但大多数儿童都不宜接种。卫生部门随后发出警告,因与提供商的沟通有误,有10多万民众可能不得不重新调整其接种第二针Moderna疫苗的日期。
与此同时,《费城询问报》的一项分析发现,相对于该州一些罕有人居住的农村地区,公共卫生机构向费城郊区——也就是梅耶的医院所在地250万居民——发放的人均疫苗数量少得多。一位州发言人对分析的方法表示质疑,但地方官员对发现结果表示赞同:在拥有56.5万人的特拉华郡,郡议会副主席莫妮卡·泰勒说,曾几何时,该郡“每周仅获得1000剂疫苗,听起来更像是电影《饥饿游戏》。”
宾州疫苗接种问题反映了众多其他大型种族和社会经济形态多样化的州在应对这个超大型复杂流程时所遇到的困境。这个全国性的举措要求在各个不对等的团队之间开展前所未有的协调工作,这些团队包括在这个充满讽刺意味的总统过渡过程中耗费了数月时间的联邦政府、资金窘迫的州和当地政府,以及由大型医疗服务提供商、小型诊所以及美国财富500强药房和百货连锁店拼凑起来的网络,它们都在疲于应对不断变化——通常是相冲突的分配和资质法规。
然而,宾州的疫苗接种问题尤为突出,其中一些是自身的问题。与其他州不一样的是,宾州拒绝创建一个集中化的疫苗接种系统,而是让居民个人来承担疫苗接种预约这个异常复杂的难题。州与地方领导人之间存在的各种官僚主义、配送问题以及冲突进一步放慢了疫苗接种进程,将各自为政的风险暴露无遗。截至3月底,宾州疫苗接种的多个指标均有所改善。然而,该州未能有效地照顾到那些最为脆弱的人群,包括黑人和拉美裔居民。
反复出现的问题让医生、地方官员和公共卫生专家对繁琐的手续以及协调的缺乏感到失望。匹兹堡黑人平等联盟成员、匹兹堡大学医学中心 McKeesport医疗系统家庭医学项目主任特雷西·康提说:“事实在于,宾州没有一个集中化的流程,这意味着人们只能依靠各个组织自行其是,并寄希望于这种模式能够奏效。它带来了诸多的不确定因素,而且让人沮丧不已。”
宾州官员也承认存在上述问题。卫生局局长阿里森·毕姆向《财富》透露,宾州经历了“死亡审判月。我们还有很多要改善的地方,但我们唯一希望的就是继续前行。”
宾州最引人注目的疫苗丑闻超出了该州的管辖范围,但它依然充斥着整个疫苗接种过程。1月,从联邦政府直接获得疫苗供应的费城让一家未经证实的初创企业Philly Fighting COVID来经营其首个大规模疫苗接种诊所。该公司创始人安德烈·多罗辛是德雷塞尔大学22岁的神经科学毕业生,他在疫情初期成为了当地的创业英雄,当时,他与朋友一道用3D打印技术为当地医院打印面罩。随后,他的初创企业(一开始是一家非营利性机构)赢得了费城卫生部门19.4万美元的合约,在服务低下的城市周边经营新冠病毒测试站点。
然而,公共媒体机构WHYY开展的一项调查称,当费城要求该公司接手城市的疫苗接种服务诊所时,这家公司突然抛弃了其位于黑人和拉美裔聚居地的测试站点。WHYY还报道称,这家初创企业在没有通知该市官员的情况下,注册了一家盈利公司。为了完成其从英雄到恶棍的公开转型,多罗辛被人发现(后自己承认)将疫苗带回家供朋友注射。当时,有资质的费城民众却被拒之其诊所门外。(多罗辛通过一名发言人表示,拒绝对此置评。该发言人还称,“我们没有同时开展测试和疫苗接种服务的资源”,但“事后我们认为停止测试是一个错误”。)
宾州大学护理学院副教授阿里森·布特海姆(新冠疫情科学专家联合组织Dear Pandemic的联合创始人)说:“我希望看到地方、郡和州层面的政府都能正确行事。在另一个宇宙,Philly Fighting COVID本应成为费城的一道最靓丽风景线。”
费城的检察长亚历山大·德桑提斯在3月发表的一篇报道称,然而在当前的宇宙,费城的计划“为城市带来了很大的风险。”(该市卫生部门的一位发言人拒绝置评。)
依然在调查这个问题的德桑提斯说:“我们的政府仓促行事,试图迅速对这个问题做出响应。这是个有问题的流程。”

这桩丑闻是宾州早期的丑事,它凸显了一个在全美普遍存在的问题:政府缺乏有经验的疫苗接种合作方。这项业务明显应该是医院和大型医疗机构提供商的工作,但这些机构自身也存在不少问题。疫情加剧了其中期预算和人手短缺问题。总的来看,大型医疗系统去年每天的损失高达近10亿美元。费城一家顶级医院的高级医师称:“前往社区注射疫苗的成本非常昂贵,这个过程需要大量的物流,同时还需要空间和招聘人手,而且医疗系统还不一定能赚到钱。”
由联邦资助的社区医疗中心可能最适合给少数族裔和服务低下的人群接种疫苗,但这些群体称,扩张这一服务的前提就是政府给他们分配更多的疫苗。
填补这一空白的是那些大型零售连锁药店,它们在此前每年令人不安的流感疫苗接种过程中积累了大量的经验。巴克莱银行(Barclays)称,仅沃尔格林和CVS预计今年就会接种全美约25%的新冠疫苗。这些连锁店在交付疫苗方面还拥有更加强劲的经济动力。它们预计疫苗接种本身将带来营收增长:这些收入来自于政府或保险公司支付的每次注射费用;来自于向进店注射的客户推销更多的物品;来自于因营销目的而收集的客户数据。这些连锁店还称,农村和种族多元化人群更容易接触到这些连锁店。CVS Caremark首席医疗官斯瑞·查古图鲁称,85%的美国民众居住在CVS药房10英里范围之内,而且称该公司在“店面位置的选择方面曾进行过一番深思熟虑”,尤其在决定每个州的哪些药房能够获得疫苗供应时十分注重平等性。
在宾州,协调这些合作伙伴的速度尤其缓慢,部分原因在于领导的更换。1月19日,拜登总统任命宾州卫生部部长蕾切尔·莱文担任美国卫生部助理部长。这一任命是历史性的:儿科医生莱文随后成为了美国参议院首位公开身份的跨性别官员。然而,此举却让莱文的家乡州宾州感到越发困惑。
州长汤姆·沃尔夫任命其时任副幕僚长阿里森·毕姆担任宾州卫生部代理部长。毕姆曾一直参与制定该州的疫苗策略,但她向《财富》透露,自己在应对疫苗供不应求的局面时已经习惯了“缺乏必要规划”的做法,以及随之而来的疫苗分配“缺乏控制”的现象。(莱文的知情人士称,这位性格外向的部长“采取了一切可行的办法来制定一个强有力的疫苗接种计划”,但“毫无疑问的是,初期阶段过后还需要对其进行改进。”)
沃尔夫和毕姆已经创建了一个两党立法工作组,得到了一些地方提供商的赞许,他们认为此举提升了疫苗接种的沟通频率和信息清晰度。宾州社区医疗中心协会政策与合作伙伴关系主任埃瑞克·吉尔说:“沟通频率在过去4-5周中增加了10倍。”宾州社区医疗中心的成员致力于为近100万得不到足够服务的居民提供医疗服务。然而,“此举并未改变这个大问题。每个人都在询问和索要疫苗,但我们手头就是没有疫苗。”
2月,该州还与波士顿咨询集团(Boston Consulting Group)签署了一项价值1160万美元的合约,帮助改善其疫苗分发服务。该集团曾帮助宾州精简了毕姆所称的“笨重的提供商网络”,该网络由获得疫苗配送的医生和药房构成。同时,波士顿咨询集团还升级了毕姆口中“异常神秘”的数据报告流程,并帮助毕姆解决了“需求大潮”问题,因为当时宾州曾发出警告,有10万居民可能无法及时获得其Moderna疫苗的第二针注射。(宾州援引了疾控中心的指引,要求接受第二针疫苗注射的居民等待高达42天,而不是通常的28天。)
毕姆说:“我们一直在搭建最根本的基础设施,同时还得应对这些紧急情况。”如今,“我们让形势变得更加紧迫。”
自初期的失利之后,宾州也取得了一些进步。截至3月25日,宾州在全美大众疫苗分发领域已经跻身前25之列。疾控中心称,超过81%的供应得到了注射,超过了全美78%的平均水平,其中28%的州居民已经获得了至少一针疫苗注射。3月31日,毕姆宣布,费城之外的所有成人在4月19日之后都可以注射疫苗(不过,城市中的居民可能得等到5月1号之后)。
然而此次疫苗接种工作在一些社区做得并不够深入,尤其是有色人种社区,而这些人群受疫情的影响尤为严重。美国疾控中心称,截至3月中旬,向费城以外地区提供的宾州疫苗仅有3%流向了黑人居民,而黑人却占到了该州非宾州当地人人口的7.5%。类似的不一致性也影响了规模较小的拉美裔和亚洲人群。这些数字并不能说明整个疫苗接种的格局,因为疾控中心掌握的种族数据仅占全美已接种人群的53%。然而,在这个宾州看似做得不甚理想的领域,整个美国也是不尽人意:在至少已经接种了一针疫苗的美国民众中,8.2%是黑人,9.3%为拉美裔;然而黑人和拉美裔占美国总人口的比例分别为13.4%和18.5%。
费城44%的人口都是黑人,不公平现象也是司空见惯。总部位于宾州哈里斯堡的药房连锁Rite Aid是该市主要的疫苗配送商,其在线注册系统理论上是面向所有居民开放。在3月底,市政府数据显示,83%的Rite Aid疫苗接种者是白人,而且药房接种白人与黑人的比例为11:1。问题在于:Rite Aid超过半数的疫苗流向了自驾前往市区的郊区居民,而这是符合宾州规定的。
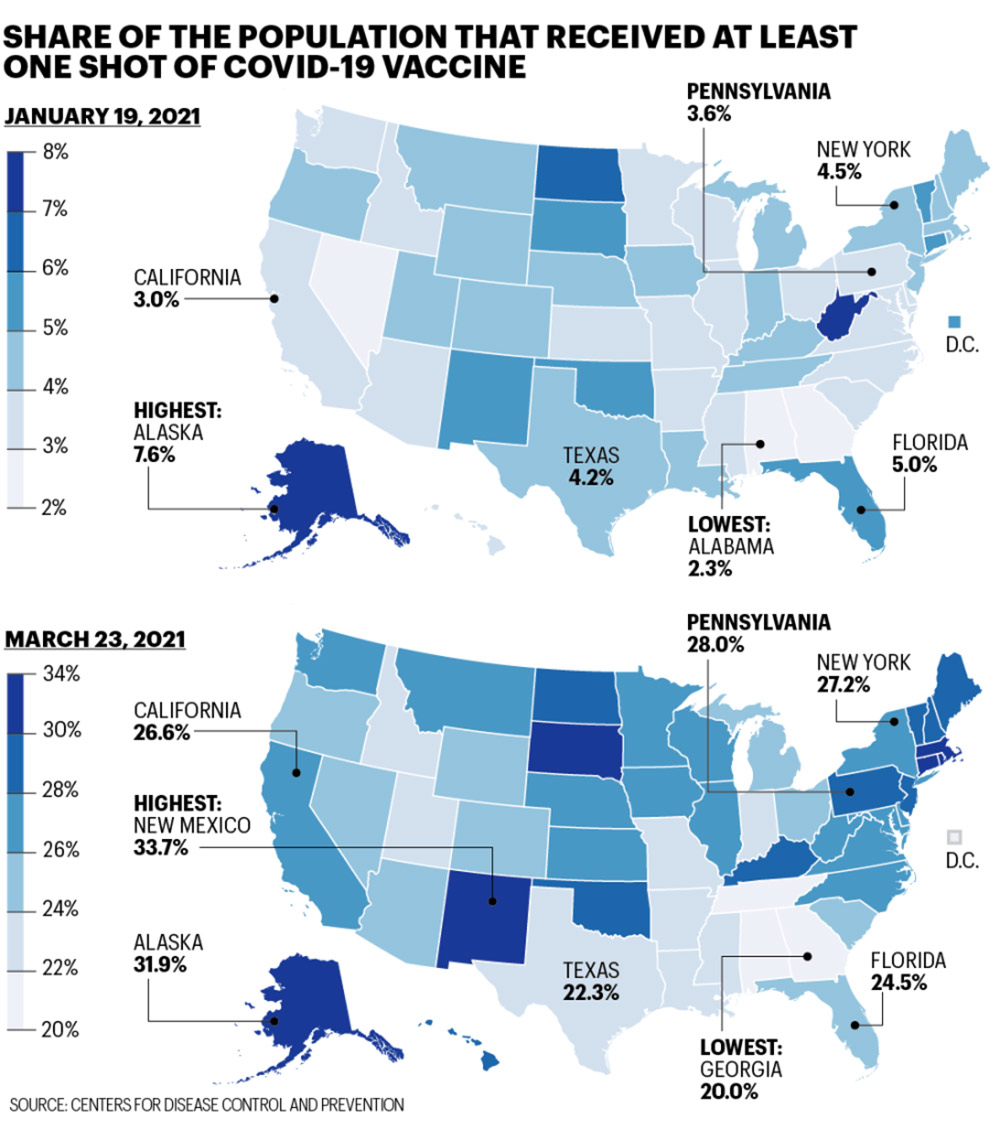
至少接种一针新冠疫苗的人口比例。来源:美国疾控中心
Rite Aid发言人称,公司已经在过去一个月提升了流向宾州黑人居民的疫苗数量比重,而且将“尽其所能地解决引发接种不平等现象的众多不一致问题。”一些因素确实已经超出了其控制范围,例如郊区居民的侵入,这一点也部分解释了为什么全美各大机构都无法解决疫苗注射的公平性。黑人和棕色人种群体更有可能是低收入人群,而且不大可能有机会接触到能够将其纳入接种序列的医疗服务提供商。他们从事“必要性”、非远程工作的可能性更大。所有这些因素为这些人通过系统进行接种预约设置了障碍,但这个系统却为可以访问互联网的人,为能够居家工作的人,为那些在一天之内有自由时间数次刷新预约网站的人提供了特权。
创建了费城“黑人医生新冠疫情联盟”的儿科外科医生阿拉·斯坦福德说,为了克服这些不一致性,“光说‘我把一个链接放在了郡网站上’是不够的,因为人们基本上看不到这个链接。”自1月以来,她的非盈利机构已经接种了3万多名费城民众;超过80%的接种人群是有色人种。该联盟的上门服务诊所仅面向特定邮编地区的居民提供接种服务(通常受新冠疫情影响最严重的地区)。斯坦福德说:“所有人都承认存在医疗服务不一致的问题,而且所有人都在谈论这个话题,但没有人积极制定解决方案。”
宾州卫生部长毕姆说:“我完全同意,我们需要下大力气营造公平氛围。”为了实现这一目标,宾州开始将其8%的联邦疫苗分配额分发给非盈利性机构,像斯坦福德这样的群体,以及“致力于接触那些难以接触人群的机构”。毕姆还表示,她希望“这一比例将不断增长”。
种族不平等仅是宾州需要解决的问题之一。65岁以上人群的疫苗接种工作依然是一个挑战。不过,宾州在这一方面的数字在3月底有所改善。毕姆和沃尔夫花费了数周的时间与地方政府机构争论,如何向费城郊区发放更多的疫苗。
与此同时,宾州的个人、社区机构和私人实体应尽其所能减少民众的困惑,并让人们接种上疫苗。到3月底,克里斯汀·梅耶的Facebook团队协助人们预约了超过1.3万次的疫苗接种服务,而且梅耶甚至在考虑这个论坛在什么时候将完成其使命。
她说,宾州的疫苗接种“并不顺畅,这并非易事,而且在很多方面都处于尴尬境地。”不过,她还表示:“我觉得现在更有希望了,因为我看到人们纷纷接种上了疫苗。”(财富中文网)
本文另一个版本登载于《财富》4月/5月刊,标题为《无疫苗可用:坎坷的宾州疫苗接种进程》。
译者:冯丰
审校:夏林
在二月的一个下雪天,克里斯汀·梅耶突然意识到自己必须亲自负责宾州的疫苗接种工作。
内科医学医师梅耶在宾州费城郊区的艾克斯顿拥有一家20000病患的医院。数周以来,他一直在接听病患的电话,这些病患拥有注射新冠疫苗的资质,但无法在药房、医生办公室,或通过当地卫生部门以及州疫苗信息网站进行预约。大多数病患的岁数都超过了75岁,而且很多人难以通过各大系统在线进行注册,因为这些系统对于科技设备操作的熟练度有很高的要求。
当暴风雪来临时,梅耶取消了个人就诊预约,并要求其医师和员工在日间帮助病患注册疫苗接种。她在其医院的Facebook页面上发布了贴文,在两个小时内,有1200人向她的办公室发送邮件寻求帮助,医院服务器也因此而瘫痪。不久之后,梅耶在Facebook上创建了一个由志愿者经营的匹配服务,以便让高龄人士或其孩子或邻居,获取找寻接种服务的帮助。截至3月底,这个组织的成员超过了6万人(包括在宾州长大、身为记者且尝试帮助其当地父母接种疫苗的我本人)。当时,很少有用户在等待州发布的消息:论坛上讨论的内容全是沃尔格林(Walgreens)、CVS、Rite Aid和其他药房什么时候才会批量公布接种预约机会,以及如何最为高效地使用其通常令人抓狂的预约网站。
梅耶通过视频向《财富》杂志透露:“说真的,疫苗接种事务让我感到心力交瘁。”她的语速和手势逐渐加快,并透露出一种沮丧情绪。“我把所有的希望和所有病患的希望都寄托在了卫生部门的身上,因为事情本该如此,然而这个流程出了问题。”
梅耶和数百万宾州民众意识到,宾州的疫苗接种问题远非令人困惑的注册流程那么简单。拥有超过2.48万家医院的宾州是全美新冠疫情死亡人数排名第五的州,同时也是美国疫苗接种问题最严重的州之一。《贝克尔医院评论对疾控中心数据的分析显示,在1月底,宾州收到了近200万剂疫苗,但仅接种了42%,在美国排名第49位,仅位于阿拉巴马之前。该州240万老年易感人群一直在想方设法获取疫苗接种服务,然而,该州却向儿科医院发送了1.2万剂疫苗,但大多数儿童都不宜接种。卫生部门随后发出警告,因与提供商的沟通有误,有10多万民众可能不得不重新调整其接种第二针Moderna疫苗的日期。
与此同时,《费城询问报》的一项分析发现,相对于该州一些罕有人居住的农村地区,公共卫生机构向费城郊区——也就是梅耶的医院所在地250万居民——发放的人均疫苗数量少得多。一位州发言人对分析的方法表示质疑,但地方官员对发现结果表示赞同:在拥有56.5万人的特拉华郡,郡议会副主席莫妮卡·泰勒说,曾几何时,该郡“每周仅获得1000剂疫苗,听起来更像是电影《饥饿游戏》。”
宾州疫苗接种问题反映了众多其他大型种族和社会经济形态多样化的州在应对这个超大型复杂流程时所遇到的困境。这个全国性的举措要求在各个不对等的团队之间开展前所未有的协调工作,这些团队包括在这个充满讽刺意味的总统过渡过程中耗费了数月时间的联邦政府、资金窘迫的州和当地政府,以及由大型医疗服务提供商、小型诊所以及美国财富500强药房和百货连锁店拼凑起来的网络,它们都在疲于应对不断变化——通常是相冲突的分配和资质法规。
然而,宾州的疫苗接种问题尤为突出,其中一些是自身的问题。与其他州不一样的是,宾州拒绝创建一个集中化的疫苗接种系统,而是让居民个人来承担疫苗接种预约这个异常复杂的难题。州与地方领导人之间存在的各种官僚主义、配送问题以及冲突进一步放慢了疫苗接种进程,将各自为政的风险暴露无遗。截至3月底,宾州疫苗接种的多个指标均有所改善。然而,该州未能有效地照顾到那些最为脆弱的人群,包括黑人和拉美裔居民。
反复出现的问题让医生、地方官员和公共卫生专家对繁琐的手续以及协调的缺乏感到失望。匹兹堡黑人平等联盟成员、匹兹堡大学医学中心 McKeesport医疗系统家庭医学项目主任特雷西·康提说:“事实在于,宾州没有一个集中化的流程,这意味着人们只能依靠各个组织自行其是,并寄希望于这种模式能够奏效。它带来了诸多的不确定因素,而且让人沮丧不已。”
宾州官员也承认存在上述问题。卫生局局长阿里森·毕姆向《财富》透露,宾州经历了“死亡审判月。我们还有很多要改善的地方,但我们唯一希望的就是继续前行。”
宾州最引人注目的疫苗丑闻超出了该州的管辖范围,但它依然充斥着整个疫苗接种过程。1月,从联邦政府直接获得疫苗供应的费城让一家未经证实的初创企业Philly Fighting COVID来经营其首个大规模疫苗接种诊所。该公司创始人安德烈·多罗辛是德雷塞尔大学22岁的神经科学毕业生,他在疫情初期成为了当地的创业英雄,当时,他与朋友一道用3D打印技术为当地医院打印面罩。随后,他的初创企业(一开始是一家非营利性机构)赢得了费城卫生部门19.4万美元的合约,在服务低下的城市周边经营新冠病毒测试站点。
然而,公共媒体机构WHYY开展的一项调查称,当费城要求该公司接手城市的疫苗接种服务诊所时,这家公司突然抛弃了其位于黑人和拉美裔聚居地的测试站点。WHYY还报道称,这家初创企业在没有通知该市官员的情况下,注册了一家盈利公司。为了完成其从英雄到恶棍的公开转型,多罗辛被人发现(后自己承认)将疫苗带回家供朋友注射。当时,有资质的费城民众却被拒之其诊所门外。(多罗辛通过一名发言人表示,拒绝对此置评。该发言人还称,“我们没有同时开展测试和疫苗接种服务的资源”,但“事后我们认为停止测试是一个错误”。)
宾州大学护理学院副教授阿里森·布特海姆(新冠疫情科学专家联合组织Dear Pandemic的联合创始人)说:“我希望看到地方、郡和州层面的政府都能正确行事。在另一个宇宙,Philly Fighting COVID本应成为费城的一道最靓丽风景线。”
费城的检察长亚历山大·德桑提斯在3月发表的一篇报道称,然而在当前的宇宙,费城的计划“为城市带来了很大的风险。”(该市卫生部门的一位发言人拒绝置评。)
依然在调查这个问题的德桑提斯说:“我们的政府仓促行事,试图迅速对这个问题做出响应。这是个有问题的流程。”
这桩丑闻是宾州早期的丑事,它凸显了一个在全美普遍存在的问题:政府缺乏有经验的疫苗接种合作方。这项业务明显应该是医院和大型医疗机构提供商的工作,但这些机构自身也存在不少问题。疫情加剧了其中期预算和人手短缺问题。总的来看,大型医疗系统去年每天的损失高达近10亿美元。费城一家顶级医院的高级医师称:“前往社区注射疫苗的成本非常昂贵,这个过程需要大量的物流,同时还需要空间和招聘人手,而且医疗系统还不一定能赚到钱。”
由联邦资助的社区医疗中心可能最适合给少数族裔和服务低下的人群接种疫苗,但这些群体称,扩张这一服务的前提就是政府给他们分配更多的疫苗。
填补这一空白的是那些大型零售连锁药店,它们在此前每年令人不安的流感疫苗接种过程中积累了大量的经验。巴克莱银行(Barclays)称,仅沃尔格林和CVS预计今年就会接种全美约25%的新冠疫苗。这些连锁店在交付疫苗方面还拥有更加强劲的经济动力。它们预计疫苗接种本身将带来营收增长:这些收入来自于政府或保险公司支付的每次注射费用;来自于向进店注射的客户推销更多的物品;来自于因营销目的而收集的客户数据。这些连锁店还称,农村和种族多元化人群更容易接触到这些连锁店。CVS Caremark首席医疗官斯瑞·查古图鲁称,85%的美国民众居住在CVS药房10英里范围之内,而且称该公司在“店面位置的选择方面曾进行过一番深思熟虑”,尤其在决定每个州的哪些药房能够获得疫苗供应时十分注重平等性。
在宾州,协调这些合作伙伴的速度尤其缓慢,部分原因在于领导的更换。1月19日,拜登总统任命宾州卫生部部长蕾切尔·莱文担任美国卫生部助理部长。这一任命是历史性的:儿科医生莱文随后成为了美国参议院首位公开身份的跨性别官员。然而,此举却让莱文的家乡州宾州感到越发困惑。
州长汤姆·沃尔夫任命其时任副幕僚长阿里森·毕姆担任宾州卫生部代理部长。毕姆曾一直参与制定该州的疫苗策略,但她向《财富》透露,自己在应对疫苗供不应求的局面时已经习惯了“缺乏必要规划”的做法,以及随之而来的疫苗分配“缺乏控制”的现象。(莱文的知情人士称,这位性格外向的部长“采取了一切可行的办法来制定一个强有力的疫苗接种计划”,但“毫无疑问的是,初期阶段过后还需要对其进行改进。”)
沃尔夫和毕姆已经创建了一个两党立法工作组,得到了一些地方提供商的赞许,他们认为此举提升了疫苗接种的沟通频率和信息清晰度。宾州社区医疗中心协会政策与合作伙伴关系主任埃瑞克·吉尔说:“沟通频率在过去4-5周中增加了10倍。”宾州社区医疗中心的成员致力于为近100万得不到足够服务的居民提供医疗服务。然而,“此举并未改变这个大问题。每个人都在询问和索要疫苗,但我们手头就是没有疫苗。”
2月,该州还与波士顿咨询集团(Boston Consulting Group)签署了一项价值1160万美元的合约,帮助改善其疫苗分发服务。该集团曾帮助宾州精简了毕姆所称的“笨重的提供商网络”,该网络由获得疫苗配送的医生和药房构成。同时,波士顿咨询集团还升级了毕姆口中“异常神秘”的数据报告流程,并帮助毕姆解决了“需求大潮”问题,因为当时宾州曾发出警告,有10万居民可能无法及时获得其Moderna疫苗的第二针注射。(宾州援引了疾控中心的指引,要求接受第二针疫苗注射的居民等待高达42天,而不是通常的28天。)
毕姆说:“我们一直在搭建最根本的基础设施,同时还得应对这些紧急情况。”如今,“我们让形势变得更加紧迫。”
自初期的失利之后,宾州也取得了一些进步。截至3月25日,宾州在全美大众疫苗分发领域已经跻身前25之列。疾控中心称,超过81%的供应得到了注射,超过了全美78%的平均水平,其中28%的州居民已经获得了至少一针疫苗注射。3月31日,毕姆宣布,费城之外的所有成人在4月19日之后都可以注射疫苗(不过,城市中的居民可能得等到5月1号之后)。
然而此次疫苗接种工作在一些社区做得并不够深入,尤其是有色人种社区,而这些人群受疫情的影响尤为严重。美国疾控中心称,截至3月中旬,向费城以外地区提供的宾州疫苗仅有3%流向了黑人居民,而黑人却占到了该州非宾州当地人人口的7.5%。类似的不一致性也影响了规模较小的拉美裔和亚洲人群。这些数字并不能说明整个疫苗接种的格局,因为疾控中心掌握的种族数据仅占全美已接种人群的53%。然而,在这个宾州看似做得不甚理想的领域,整个美国也是不尽人意:在至少已经接种了一针疫苗的美国民众中,8.2%是黑人,9.3%为拉美裔;然而黑人和拉美裔占美国总人口的比例分别为13.4%和18.5%。
费城44%的人口都是黑人,不公平现象也是司空见惯。总部位于宾州哈里斯堡的药房连锁Rite Aid是该市主要的疫苗配送商,其在线注册系统理论上是面向所有居民开放。在3月底,市政府数据显示,83%的Rite Aid疫苗接种者是白人,而且药房接种白人与黑人的比例为11:1。问题在于:Rite Aid超过半数的疫苗流向了自驾前往市区的郊区居民,而这是符合宾州规定的。
Rite Aid发言人称,公司已经在过去一个月提升了流向宾州黑人居民的疫苗数量比重,而且将“尽其所能地解决引发接种不平等现象的众多不一致问题。”一些因素确实已经超出了其控制范围,例如郊区居民的侵入,这一点也部分解释了为什么全美各大机构都无法解决疫苗注射的公平性。黑人和棕色人种群体更有可能是低收入人群,而且不大可能有机会接触到能够将其纳入接种序列的医疗服务提供商。他们从事“必要性”、非远程工作的可能性更大。所有这些因素为这些人通过系统进行接种预约设置了障碍,但这个系统却为可以访问互联网的人,为能够居家工作的人,为那些在一天之内有自由时间数次刷新预约网站的人提供了特权。
创建了费城“黑人医生新冠疫情联盟”的儿科外科医生阿拉·斯坦福德说,为了克服这些不一致性,“光说‘我把一个链接放在了郡网站上’是不够的,因为人们基本上看不到这个链接。”自1月以来,她的非盈利机构已经接种了3万多名费城民众;超过80%的接种人群是有色人种。该联盟的上门服务诊所仅面向特定邮编地区的居民提供接种服务(通常受新冠疫情影响最严重的地区)。斯坦福德说:“所有人都承认存在医疗服务不一致的问题,而且所有人都在谈论这个话题,但没有人积极制定解决方案。”
宾州卫生部长毕姆说:“我完全同意,我们需要下大力气营造公平氛围。”为了实现这一目标,宾州开始将其8%的联邦疫苗分配额分发给非盈利性机构,像斯坦福德这样的群体,以及“致力于接触那些难以接触人群的机构”。毕姆还表示,她希望“这一比例将不断增长”。
种族不平等仅是宾州需要解决的问题之一。65岁以上人群的疫苗接种工作依然是一个挑战。不过,宾州在这一方面的数字在3月底有所改善。毕姆和沃尔夫花费了数周的时间与地方政府机构争论,如何向费城郊区发放更多的疫苗。
与此同时,宾州的个人、社区机构和私人实体应尽其所能减少民众的困惑,并让人们接种上疫苗。到3月底,克里斯汀·梅耶的Facebook团队协助人们预约了超过1.3万次的疫苗接种服务,而且梅耶甚至在考虑这个论坛在什么时候将完成其使命。
她说,宾州的疫苗接种“并不顺畅,这并非易事,而且在很多方面都处于尴尬境地。”不过,她还表示:“我觉得现在更有希望了,因为我看到人们纷纷接种上了疫苗。”(财富中文网)
本文另一个版本登载于《财富》4月/5月刊,标题为《无疫苗可用:坎坷的宾州疫苗接种进程》。
译者:冯丰
审校:夏林
It was a February snow day that made Christine Meyer snap—and realize she had to take Pennsylvania’s vaccine rollout into her own hands.
Meyer, an internal medicine physician who owns a 20,000-patient practice in Exton, Pa., in the Philadelphia suburbs, had spent weeks fielding calls from patients who were eligible for COVID-19 vaccines but who couldn’t find an appointment—at pharmacies, at doctors’ offices, via local health departments, or through the state’s vaccine-information website. Most of them were over 75, and many struggled to register online through systems that required tech savvy.
When a snowstorm hit, canceling in-person appointments, Meyer asked her clinicians and staff to spend the day helping patients register for jabs. She posted about it on her practice’s Facebook page—and within two hours she had 1,200 people emailing her office for help, crashing her servers. Soon Meyer created a volunteer-run matchmaking service on Facebook, allowing seniors—or their children or neighbors—to request help finding a vaccine. As of late March, the group had more than 60,000 members (including this Pennsylvania-raised reporter, trying to help her local parents). By then, few users were waiting to hear from the state: The forum was dominated by talk about when Walgreens, CVS, Rite Aid, and other pharmacies were releasing blocks of appointments, and how best to navigate their often-maddening websites.
“This vaccine thing honestly bowled me over,” Meyer told Fortune via video, her voice and hand gestures speeding up with frustration. “I put all of my faith, and all of my patients’ faith, in the health department—because that’s how it was supposed to work. But the process is broken.”
As Meyer and millions of Pennsylvanians have learned, the state’s vaccine-rollout problems run far deeper than a confusing sign-up process. The Keystone State, with more than 24,800 fatalities, is the state with the fifth-highest COVID-19 death toll. It also has one of the nation’s longest litanies of vaccine stumbles. At the end of January, Pennsylvania had received nearly 2 million doses but had distributed only 42%—ranking the state 49th, ahead of onlyAlabama, according to a Becker’s Hospital Review analysis of CDC data. As the state’s 2.4 million seniors scrambled to find vaccines for a disease they are particularly vulnerable to, the state sent 12,000 doses to pediatric offices—even though most children aren’t yet eligible for shots. The health department later warned that more than 100,000 people might have to reschedule their second appointments for the two-dose Moderna vaccine because of miscommunication with providers.
Meanwhile, public health authorities were sending far fewer doses per capita to the 2.5 million residents of the Philadelphia suburbs—Meyer’s territory—than to some of the state’s sparsely populated rural enclaves, a Philadelphia Inquirer analysis found. A state spokesperson disputes the analysis’s methods, but local officials echo its findings: At one point, says Monica Taylor, council vice chairperson of 565,000-person Delaware County, the county was “getting only 1,000 doses a week. It made it more like the Hunger Games.”
Pennsylvania’s rollout problems have mirrored those of many other large, racially and socioeconomically diverse states as they navigate a massively complex process. The national effort has required unprecedented coordination among a mismatched team of players, including a federal government that squandered months in an acrimonious presidential transition; cash-strapped state and local governments; and a patchwork of big health care providers, small clinics, and Fortune 500 pharmacy and grocery chains sorting through changing—and often conflicting—distribution and eligibility rules.
Still, Pennsylvania’s campaign has stood out for its problems, some of which are self-inflicted. Unlike some of its peers, Pennsylvania declined to create a centralized vaccination system, putting the burden on individual residents to navigate the appointment maze. A host of bureaucratic complications, distribution failures, and conflicts between state and local leaders have slowed things down even more—showing the danger of an every-party-for-itself approach. By late March, Pennsylvania had improved its rollout by several metrics. But it continues to struggle to reach its most vulnerable populations, including Black and Latinx residents.
The persistent problems have left doctors, local officials, and public health experts lamenting an excess of red tape and a lack of coordination. “The fact that there’s not a centralized process across the state means that you’re really depending on each individual organization doing their own thing and hoping that it works,” says Tracey Conti, a member of the Pittsburgh-based Black Equity Coalition and program director of family medicine at the UPMC McKeesport health care system. “It creates a lot of unknowns—and a lot of frustration.”
State officials acknowledge as much. Pennsylvania has gone through “a month of reckoning,” acting Health Secretary Alison Beam tells Fortune. “There is a lot of room to improve—and we only want to be moving forward.”
Pennsylvania’s most headline-grabbing vaccine scandal wasn’t within the state’s control—but it continues to resonate across its rollout. In January, the city of Philadelphia, which gets its vaccine supply directly from the federal government, asked an unproven startup called Philly Fighting COVID to run its first mass vaccination clinic. Founder Andrei Doroshin, a 22-year-old neuroscience grad student at Drexel University, had become a local entrepreneurial hero in the early days of the pandemic, recruiting friends to 3-D print face shields for local hospitals. Then his startup, which initially operated as a nonprofit, won a $194,000 contract from Philadelphia’s health department to operate COVID-19 testing sites in underserved city neighborhoods.
But once it was asked to run the city’s vaccination clinic, Philly Fighting COVID abruptly abandoned its testing commitments in predominantly Black and Latinx neighborhoods, according to an investigation by public-media organization WHYY—which also reported that the startup had, without informing city officials, registered a for-profit arm. To complete his public transformation from hero to villain, Doroshin was seen—and later admitted to—taking home vaccine doses for his friends, on a day when eligible Philadelphians were shut out at his clinic. (Doroshin declined to comment through a spokesperson, who said that “we didn’t have the resources to do testing and vaccinations at the same time,” but “it was a mistake in hindsight” to stop testing.)
“I love reading about governments—on a local, county, and state level—that are getting it right. And in an alternate universe, Philly Fighting COVID could have been the best thing that happened to Philadelphia,” says Alison Buttenheim, an associate professor at the University of Pennsylvania School of Nursing (and a co-founder of the “Dear Pandemic” collective of COVID-19 scientific experts).
But in this universe, Philadelphia’s plan “placed the city at great risk,” a March report from city Inspector General Alexander DeSantis found. (A spokesperson for the city health department declined to comment.)
“Our government was working in a hurry and trying to respond to something really quickly,” says DeSantis, who is continuing to investigate the affair. “It was a process that broke.”
The scandal was an early black eye for Pennsylvania, and it highlighted a common problem nationwide—the lack of established vaccine partners for governments. Hospitals and large health care providers might seem like obvious distributors, but they face problems of their own. The pandemic exacerbated their enduring budget and personnel crunches; collectively, large health care systems were estimated to be losing almost $1 billion a day last year. “It’s expensive to go out there in the community and put shots in arms,” says a senior physician at a top Philadelphia hospital. “It requires a lot of logistics, space, and hiring people—and it’s not necessarily going to make a health system money.”
Federally funded community health centers may be best positioned to vaccinate minority and underserved populations, but those groups say they need bigger allocations of vaccines from governments to scale up.
Into this vacuum have stepped the large retail pharmacy chains—already experienced at distributing yearly flu shots. Walgreens and CVS alone are expected to give out about 25% of COVID shots nationwide this year, according to Barclays. Those chains also have stronger economic incentives around delivering vaccines. They expect revenue growth from the rollout itself—from government or insurance payments per shot; from selling more stuff to customers who come in for shots; and from collecting customers’ data for marketing purposes. The chains also claim to be more accessible to rural and racially diverse populations. CVS Caremark chief medical officer Sree Chaguturu notes that 85% of Americans live within 10 miles of a CVS pharmacy, and says that the company has tried to “be really thoughtful on store locations,” especially in terms of equity, when making decisions about which pharmacies in each state get its supply of vaccines.
In Pennsylvania, coordination among these partners was especially slow to jell—owing in part to a change in command. On Jan. 19, President Biden appointed Rachel Levine, the state secretary of health, to be U.S. assistant secretary of health. The nomination was historic: Levine, a pediatrician, later became the first openly transgender official confirmed by the U.S. Senate. But it only added to the confusion in her home state.
Gov. Tom Wolf appointed his then deputy chief of staff, Alison Beam, as acting secretary of health. Beam had been involved in the state’s vaccine strategy, but she tells Fortune that she inherited “a lack of the necessary planning” for dealing with demand that outpaced supply, and a resulting “lack of controls” in how to allocate vaccines. (A source close to Levine says that the outgoing secretary “did everything feasible to put together a robust vaccine plan” but that “there’s no question improvements needed to be made after the initial phase.”)
Wolf and Beam have created a bipartisan legislative task force, which some local providers praise for increasing the frequency and clarity of information around the rollout. “The communication has increased tenfold over the past four to five weeks,” says Eric Kiehl, director of policy and partnership at the Pennsylvania Association of Community Health Centers, whose members provide health care to nearly 1 million underserved residents. But “that doesn't change the big issue. Everybody’s calling and wanting vaccine, and we just don’t have it.”
In February, the state also gave Boston Consulting Group an $11.6 million contract to help improve its vaccine distribution. BCG has helped Pennsylvania pare down what Beam calls “an unwieldy provider network” of doctors and pharmacies who have been allocated vaccines, and it’s upgrading what Beam says is the state’s “undoubtedly arcane” data-reporting process. It also helped Beam work through a “tidal wave” of requests when the state warned that up to 100,000 residents might not get their second Moderna shots in time. (Citing CDC guidance, Pennsylvania addressed the shortage by asking residents to wait up to 42 days for their second shots, instead of the more usual 28.)
“We were working on the foundational infrastructure” and “simultaneously responding to these fires,” Beam says. Now, “we are driving the urgency.”
Since those early days, Pennsylvania has made up some ground. As of March 25, the state had climbed into the top half of states for vaccine distribution among the general population. More than 81% of its supply has been administered, according to the CDC, surpassing the national average of 78%, and 28% of state residents had received at least one dose. And on March 31, Beam announced that all adults outside of Philadelphia would be eligible for a vaccine by April 19 (although those in the city may have to wait until May 1).
But the rollout hasn’t penetrated far enough into some communities—especially communities of color, which have been disproportionately harmed by the pandemic. By mid-March only 3% of Pennsylvania’s vaccines outside Philadelphia had gone to Black residents, according to the CDC, even though Black people account for 7.5% of the state’s non-Philly population; similar disparities affect the smaller Latinx and Asian populations. These numbers don’t paint a complete picture, since the CDC has racial data available for only 53% of national vaccine recipients. Still, Pennsylvania seems to be underdelivering on a front where the nation already does poorly: Of Americans who have had at least one dose, 8.2% are Black and 9.3% are Latinx; while the U.S. population as a whole is 13.4% Black and 18.5% Latinx.
In Philadelphia, whose population is 44% Black, the inequities are just as stark. Rite Aid, the pharmacy chain based in Harrisburg, Pa., is one of the city’s dominant distributors, with an online registration system that’s theoretically equally open to all residents. In late March city government data showed that 83% of Rite Aid’s vaccine recipients were white, and that the pharmacy had inoculated nearly 11 white people for every Black person who received a shot. One problem: More than half of Rite Aid shots went to suburban residents who drove into the city—which is permissible under state guidelines.
A Rite Aid spokesperson says the company has increased the share of vaccine doses going to Black Pennsylvanians within the past month, and is “working tirelessly to overcome the many disparities” that cause vaccine inequity. Some factors are indeed outside its control, like the suburbanite invasion—which also illuminates some of the reasons why authorities nationwide are flunking vaccine equity. Black and brown people are more likely to be lower-income and less likely to have access to health care providers who can steer them into the vaccination pipeline. They’re also more likely to work in “essential,” non-remote jobs. All those factors create barriers to getting vaccine appointments through systems that privilege people with Internet access, the ability to work from home, and the free time to refresh scheduling websites multiple times a day.
To overcome these disparities, “it’s not enough to say, ‘I put a link out on a county website,’ where it was in essence buried,” says Ala Stanford, the pediatric surgeon who founded Philadelphia’s Black Doctors COVID-19 Consortium. Since January, her nonprofit has vaccinated more than 30,000 Philadelphians; more than 80% of the recipients are people of color. The organization runs walk-up clinics that administer shots only to residents of specific zip codes (usually those hardest-hit by COVID). “Everyone acknowledges the health disparities. And everybody talks about it—but no one makes an active plan,” Stanford says.
“I absolutely agree that we need to make inroads on equity,” says Beam, the health secretary. To do so, the state has started dedicating 8% of its federal vaccine allocations to nonprofits, groups like Stanford’s and “entities that show that they are reaching hard-to-reach populations,” Beam says, adding that she hopes “that share will be ever-increasing.”
50%+
SHARE OF VACCINES FROM PHILADELPHIA RITE AID PHARMACIES THAT HAVE BEEN DISTRIBUTED TO PEOPLE WHO LIVE OUTSIDE THE CITY. SOURCE: RITE AID
50%+
Racial equity is only one of the puzzles the state needs to solve. Access has also been a challenge for those 65 and older, although Pennsylvania’s numbers there had improved by the end of March. And Beam and Wolf have spent weeks embroiled in arguments with local authorities over how to increase distribution of vaccines to the Philadelphia suburbs.
In the meantime, individuals, community organizations, and private entities all over the state do what they can to cut through the confusion and get jabs in arms. By late March, Christine Meyer’s Facebook group had facilitated more than 13,000 vaccine appointments—and Meyer was even contemplating the day when the forum might no longer be needed.
Pennsylvania’s rollout is “not smooth, it’s not easy, it’s embarrassing in a lot of ways,” she says. Still, she adds, “I feel more hopeful—because I see people getting vaccines.”
A version of this article appears in the April/May issue of Fortune with the headline, "Missing their shot: A rocky rollout in Pennsylvania."






